Cardiovascular disorders
Cardiovascular disorders are conditions of the heart and blood vessels including various heart, stroke and vascular diseases.
There can be a number of precipitating factors that result in cardiovascular disease, however the main underlying factor is atherosclerosis or the gradual build up of fatty deposits in the blood vessels. When these vessels become ‘clogged’ and narrowed the supply of blood flow to the brain, heart and other vital organs is affected.
Symptoms and characteristics:
Typical symptoms of cardiovascular disorders include:
- chest pain
- cyanosis or a bluish discolouration of the fingertips
- swelling or puffiness in the lower legs and feet
- dyspnea which is a shortness of breath and difficulty breathing
- palpitations which is an irregular, fluttering or skipping heartbeat
- decreased endurance and easily fatigued
- syncope which includes fainting, dizziness or a brief loss of consciousness.
types of cardiovascular disorders:
- Chronic pulmonary heart disease
- Congenital heart disease
- Coronary heart disease
- Haemophilia
- High blood pressure
- Peripheral vascular disease
- Raynaud's phenomenon
- Stroke
- Thalassemia
Non-invasive vascular laboratory
Features of the non-invasive vascular laboratory
include:
·
Staff of 23 physicians, 24 vascular technologists, and one research
technologist. Each study is reviewed and interpreted by either a vascular
medicine physician or a vascular surgeons.
· Two fully functional vascular laboratories are available for patient care.
Diagnostic machines have portable capability to meet the needs of the entire
Cleveland Clinic patient population.
· The lab is committed to meet the needs of patients and staff, including
patients involved in research studies and outside physician referrals. One
ultrasound machine is dedicated to research.
· Digital image management sets us apart from all vascular laboratories in
terms of information processing and accuracy. Computer workstations allow the
immediate transfer of digital information at the time of examination and makes
physician review of critical images more readily available. This system allows
for review of duplex ultrasound examinations, arteriography, MRI and CT scans.
This enables a direct comparison of different modalities of imaging for better
and quicker correlation and quality assurance.
·
Continuing education and a commitment to state-of-the-art technology
allows for a knowledgeable and well-trained staff.
Studies performed in the non-invasive vascular
laboratory include:
· Renal artery ultrasound
· Aorta and peripheral artery ultrasound
· Pulse volume recordings/ABI of the upper and lower extremities
· Exercise and treadmill testing of both upper and lower extremities (respectively)
· Venous ultrasound of both the upper and lower extremities
· Venous reflux testing
· Vein mapping
· Arterial mapping studies
· Upper and lower extremity graft surveillance
· Intra-operative duplex ultrasonography
· Venous plethysmography
· TCP02 testing
Cardiac arrhythmia
Cardiac arrhythmia is the condition in which the heart's normal rhythm is disrupted.
In this article, we describe the heart's normal sinus rhythm and a number of
different types of disruptions of this rhythm and how dynamical systems can be used to understand the behavior
of the heart in these circumstances.
The heart pumps blood
containing oxygen, nutrients, immune cells, and regulatory molecules to the
body organs. The rhythm of the heart is set by a small region of cardiac muscle
cells in the right atrium called the sinoatrial (SA) node that acts as a
spontaneous pacemaker, but is under the control of nerves and circulating
hormones that affect the heart rate via a host of control circuits that
maintain adequate blood pressure and oxygenation. The heart itself is composed
of two upper chambers, the atria, and two lower chambers, the ventricles.
The normal heart rhythm is called sinus rhythm. In sinus rhythm each
beat spontaneously generated from the SA node produces a propagating wave of
bioelectricity that spreads throughout the four chambers of the heart in a coordinated
fashion. Each impulse propagates throughout the atria before being channeled
through the atrioventricular (AV) node to the ventricles. This electrical wave
triggers intracellular calcium processes that produce the contractions of the
cardiac muscle that pump the blood to the organs of the body. The slow (about
120-200 ms) conduction time through the AV node allows adequate
time for atrial contraction and ventricular filling. Upon emerging from the AV
node, the electrical impulse propagates through specialized conducting bundles
called the His-Purkinje system and from there to the ventricles. The
His-Purkinje system allows rapid conduction to all areas of the ventricles and
therefore is responsible for ensuring effective ventricular contraction. Normally,
the heart beats at a rate of approximately 75 beats per minute (although there
is substantial individual variation) and pumps about 5 liters of blood per
minute.
The heart rhythm is
typically monitored by an electrocardiogram (ECG), which measures the voltage
differences between points on the surface of the body.
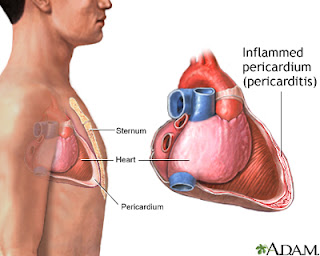
Pericarditis
Pericarditis is a condition in which the sac-like covering
around the heart (pericardium) becomes inflamed.
Causes
Pericarditis is usually a complication of viral infections, most
commonly echovirus or coxsackie virus. Less frequently, it is caused by
influenza or HIV infection.
Infections with bacteria can lead to bacterial pericarditis
(also called purulent pericarditis). Some fungal infections can also produce
pericarditis.
In addition, pericarditis can be associated with diseases such
as:
- Autoimmune disorders
- Cancer
(including leukemia)
- HIV infection and AIDS
- Hypothyroidism
- Kidney failure
- Rheumatic fever
- Tuberculosis
Often the cause of pericarditis remains unknown. In this case,
the condition is called idiopathic pericarditis.
Pericarditis most often affects men aged 20 - 50. It usually
follows respiratory infections. In children, it is most
commonly caused by adenovirus or coxsackie virus.
Symptoms
- Ankle, feet, and leg
swelling (occasionally)
- Anxiety
- Breathing difficulty
when lying down
- Chest pain,
caused by the inflamed pericardium rubbing against the heart
- May
radiate to the neck, shoulder, back, or abdomen
- Often
increases with deep breathing and lying flat, and may increase with
coughing and swallowing
- Pleuritis type: a sharp, stabbing pain
- Usually
relieved by sitting up and leaning forward
- Dry cough
- Fatigue
- Fever
- Need to
bend over or hold the chest while breathing
Treatment
The cause of pericarditis must be identified, if possible.
Medications include:
- Analgesics for pain
- Antibiotics
for bacterial pericarditis
- Antifungal
medications for fungal pericarditis
- Aspirin
or a nonsteroidal anti-inflammatory drug (NSAID) such as ibuprofen for
inflammation of the pericardium
- Corticosteroids
such as prednisone (in some patients)
- Colchicine
If the buildup of fluid in the pericardium makes the heart
function poorly or produces cardiac tamponade,
it is necessary to drain the fluid from the sac. This procedure, called
pericardiocentesis, may be done using an echocardiography-guided needle or
minor surgery.
If the pericarditis is chronic,
recurrent, or causes constrictive pericarditis, cutting or removing part of the
pericardium may be recommended.
Pericarditis can range from mild cases that get better on their
own to life-threatening cases. The condition can be complicated by significant
fluid buildup around the heart and poor heart function.
The outcome is good if the disorder is treated promptly. Most
people recover in 2 weeks to 3 months. However, pericarditis may come back.
Endocarditis
Endocarditis is an inflammation of your heart's inner lining. The most
common type, bacterial endocarditis, occurs when germs enter your heart. These
germs come through your bloodstream from another part of your body, often your
mouth. Bacterial endocarditis can damage your heart valves. If untreated, it
can be life-threatening. It is rare in healthy hearts.
Risk factors include having
- An
abnormal or damaged heart valve
- A
severe case of mitral valve prolapse
- An
artificial heart valve
- Certain
heart defects
If you have a high risk of bacterial endocarditis, your doctor might
prescribe antibiotics before dental work and certain types of surgery.
Early treatment can help you avoid complications. Symptoms you might
notice include fever, shortness of breath, fluid buildup in your arms or legs,
tiny red spots on your skin and weight loss. Treatment usually involves
high-dose antibiotics.
Rheumatic heart disease
Rheumatism:
Rheumatism is a
non-specific term used to describe medical conditions concerning joints and
connective tissue. Some conditions that were once given the general label of rheumatism or
called rheumatic diseases were later classified as rheumatoid arthritis, osteoarthritis, lupus,
fibromyalgia, and tendonitis. Autoimmune disorders, when remain
unnamed but cause pain as well as affecting other organs, were classed
as rheumatism.
Illnesses like lupus
were particularly susceptible to being called rheumatism. Later
understanding of the causes of these illnesses shows that the problem is not
dysfunction of the joints, but rather immune systems that can attack
joints, muscles and organs. The general term rheumatism is
seldom heard now in medical communities because health professionals feel that
specific naming of illnesses can better point toward standards or treatment and
care.
Rheumatic fever:
Now days, rheumatism
is commonly associated with either arthritis or rheumatic fever. Rheumatic
fever is a serious inflammatory disease that affects different areas of the
body, including the joints, heart, skin, nervous system, and brain. Rheumatic
fever may develop after a serious infection with streptococcus bacteria,
especially strep throat. It is believed to be caused by antibody cross-reactivity that
can involve the heart, joints, skin, and brain. The
illness typically develops two to three weeks after a streptococcal infection.
Rheumatic heart
disease:
If left untreated,
rheumatic fever can result in serious complications, including scarring of the
heart's valves and this condition is called rheumatic heart disease. The
disease can be caused by recurring rheumatic fever which can lead to scar
tissue and abnormal changes in myocardium (heart muscle). This results in
compromising the heart function to pump blood effectively throughout the body.
From rheumatic fever
to rheumatic heart disease:
In order to
understand how rheumatic heart disease manifests, it is pertinent to know what
happens when the individual experiences an episode of rheumatic fever. The
fever itself is an inflammatory disease that manifests itself as
strep in the throat. The infection in the throat can work through the
connective tissue in the body, eventually making its way to the joints,
the skin, and even the heart and the brain. Repeated episodes of rheumatic
fever can cause damage to any of the organs that are reached through the
connective tissue. In the case of the heart, the infection can cause the heart
valves to thicken, a condition which makes the enlarged valves work less
efficiently.
Cardiomyopathy
Cardiomyopathy refers to diseases of the heart muscle. These diseases
enlarge your heart muscle or make it thicker and more rigid than normal. In
rare cases, scar tissue replaces the muscle tissue.
Some people live long, healthy lives with cardiomyopathy. Some people
don't even realize they have it. In others, however, it can make the heart less
able to pump blood through the body. This can cause serious complications,
including
- Heart failure
- Abnormal heart rhythms
- Fluid buildup in your lungs or legs
- Endocarditis, an inflammation of the
heart lining
Heart attacks, high blood pressure or infections can all cause cardiomyopathy.
Some types of cardiomyopathy run in families. In many people, however, the
cause is unknown. Treatment might involve medicines, surgery, other medical
procedures and lifestyle changes.
Heart Attack
Each year over a million people in the U.S. have a heart attack. About half of them die. Many people have permanent heart damage or die because they don't get help immediately. It's important to know the symptoms of a heart attack and call 9-1-1 if someone is having them. Those symptoms include
- Chest discomfort - pressure, squeezing, or pain
- Shortness of breath
- Discomfort in the upper body - arms, shoulder, neck, back
- Nausea, vomiting, dizziness, lightheadedness, sweating
These symptoms can sometimes be different in women.
What exactly is a heart attack? Most heart attacks happen when a clot in the coronary artery blocks the supply of blood and oxygen to the heart. Often this leads to an irregular heartbeat - called an arrhythmia - that causes a severe decrease in the pumping function of the heart. A blockage that is not treated within a few hours causes the affected heart muscle to die.







.jpg)

No hay comentarios:
Publicar un comentario